Share:

The clinical application of intense pulsed light therapy for vascular skin diseases has been summarized in the previous article (see: Phototherapy Miracle Egg | Clinical Application of Intense Pulsed Light Therapy Device (1) Click on the blue text to read ←). This article will explore the clinical application of intense pulsed light in the treatment of pigmentary skin diseases
1. Treatment of superficial pigmentary lesions of the skin with intense pulsed light
Toyonobu Yamashita et al. [1] used intense pulsed light to treat facial sunspots and conducted in-depth observations and studies on the mechanism of intense pulsed light in removing skin pigmentation through reflective confocal microscopy (RCM) and optical coherence tomography (OCT).< This study selected 3 subjects with facial sunspots and treated them with intense pulsed light. The parameters were set as a 560nm filter, twin pulses, sub pulse widths of 2.8ms and 5ms, sub pulse intervals of 20ms, and energy density of 23-26J/cm ². I received a total of 3 treatments with an interval of 3 weeks< After intense pulsed light treatment, small areas of crusted pigmentation appeared on the surface of the subjects' skin. The researchers defined this melanin volume aggregation as intraepidermal microcrusts (IEMCs) of the epidermis. The morphological changes of IEMCs are shown in the following figure. On the first day after treatment, nebulous aggregates of melanin appeared in the epidermis, and gradually formed denser coagulative IEMCs by the third day. This type of IEM gradually sheds from the skin within 5-7 days, and no formation of IEM was observed on adjacent non pigmented skin.
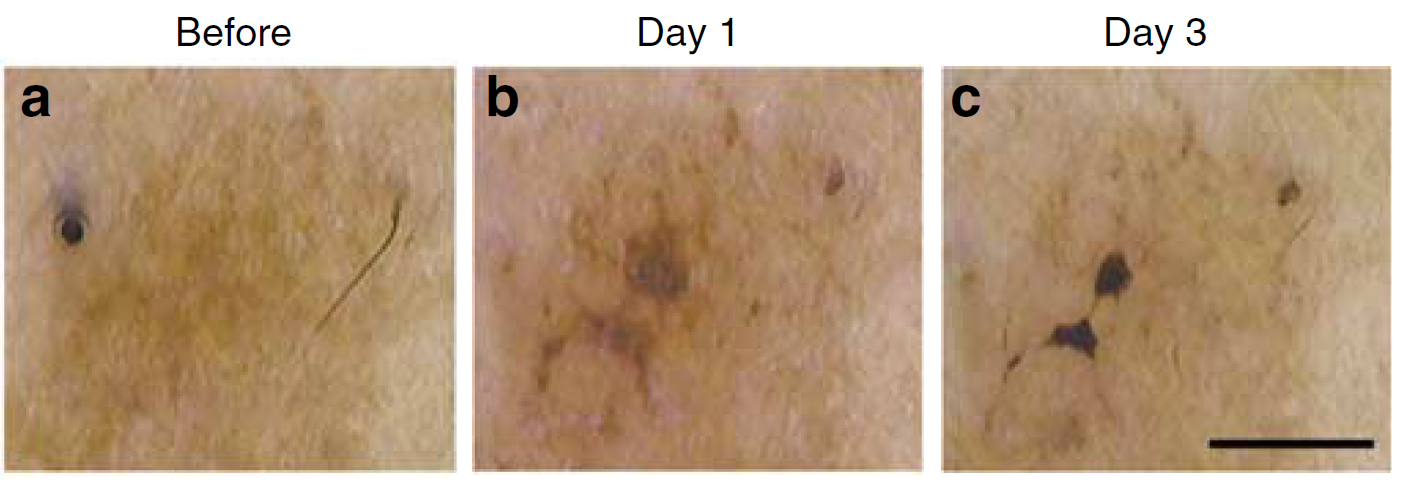
The morphological changes of IEMC after the first intense pulsed light irradiation. On the first day after treatment, IEMC appeared as a high pigment area, which gradually decreased in size by the third day until it peeled off from the skin surface< After the second and third treatments, almost all subjects had mild IEMC symptoms. After treatment, a trend of reduced pigmentation was observed in all subjects. However, the amount of pigment removal varies for each subject, which seems to depend on the degree of skin pigmentation. Observation of skin color shows a brief mild inflammation after the first intense pulsed light irradiation. The inflammatory changes disappeared after a few days without causing excessive pigmentation after inflammation
[Changes in appearance of pigmented lesions caused by intense pulsed light therapy]
Before treatment, RCM imaging clearly showed enhanced images of melanin caps in the pigmented areas, where many melanosomes (bright white spots) were clustered. Compared with the surrounding normal areas, the reflection signal of melanosomes in the colored areas was significantly higher (Figure 3a and b). After intense pulsed light irradiation, the distribution of melanosomes in RCM images underwent significant changes. After 18 hours of treatment, the collapse of the melanin cap can be seen under the microscope, and melanosomes are dispersed in the basal keratinocytes, forming a high refractive index plane and rapidly migrating to the stratum corneum of the skin before shedding. On the 5th day after treatment, a new stratum corneum appeared beneath the IEM.
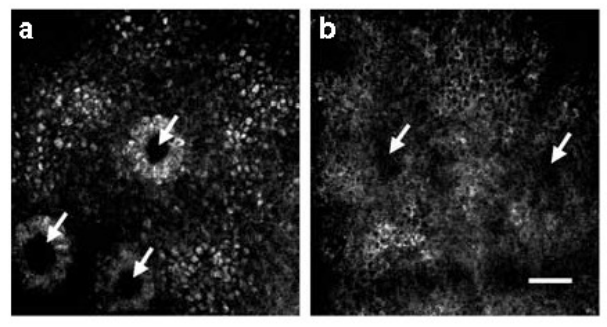
RCM image of melanin distribution before treatment. (a) Pigmentation area of sunspot. (b) Surrounding area of sunspot shown in figure (a). The backscattered light from the melanin cap (bright white spot) is higher in (a) than in (b). The arrows in both figures indicate the dermal papilla
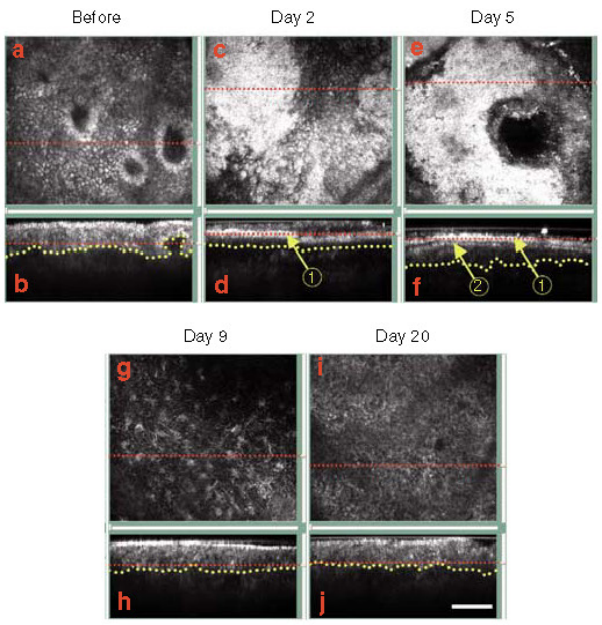
Changes in RCM images over time after the first treatment. Horizontal images (top) and vertical images (bottom) are displayed in each image, with red dashed lines indicating the corresponding planes imaged in the vertical and horizontal images, and yellow lines indicating the epidermal dermal junction. (a and b) Prior to treatment, high reflectivity of the melanin cap (bright white spots) on the epidermal basal layer nucleus can be observed. (c and d) On the second day after treatment, a high reflectivity layer (arrow 1) was observed in the RCM vertical image. (e and f) On the fifth day after treatment, as shown in the vertical image, the high reflectivity layer rapidly migrated to the skin surface. In addition, another different reflectivity layer was identified (arrow 1). On the 9th day, many melanocytes were observed in the basal layer of the horizontal image. On the 20th day, the reflectance intensity of the basal layer increased, but no melanocytes were seen
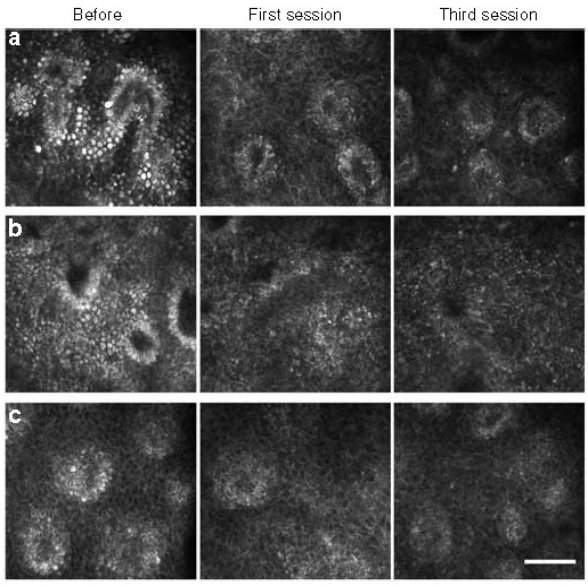
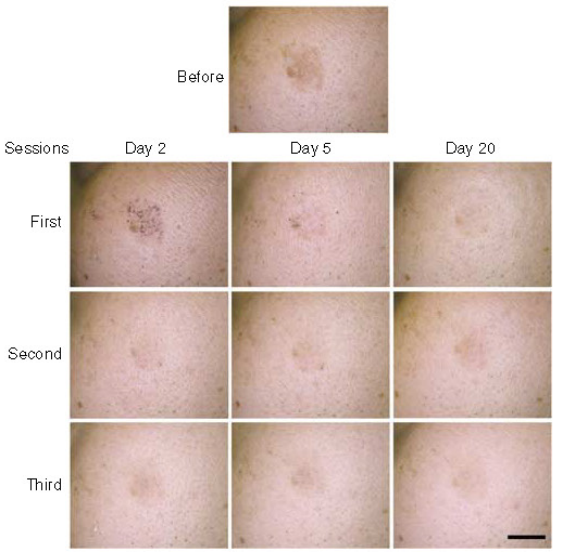
Comparison of RCM images before and after treatment. (a – c) RCM images of three subjects before and after treatment. The reflectance level of melanin in the epidermis basal layer of all subjects decreased with each treatment. From the OCT images before and after treatment, it can be seen that compared with the normal skin on the contralateral face, the OCT images of the epidermal layer at the site of sunspot pigmentation are thicker. After the second and third treatments, the epidermal thickness gradually returned to normal. After all irradiation, there was no significant change in the thickness of normal skin. OCT images can also observe rapid upward migration of IEMCs in the epidermis.
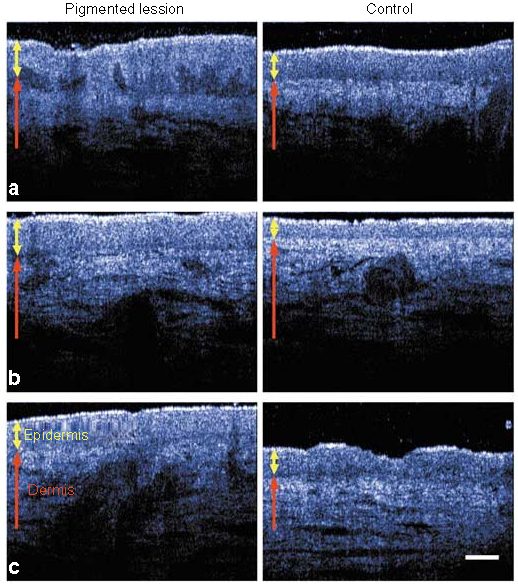
OCT imaging of sunspot epidermis. (a-c) displays OCT images of three subjects' facial sunspot areas and normal skin areas. The epidermal layer in the sunspot area is thicker than that in the normal skin area
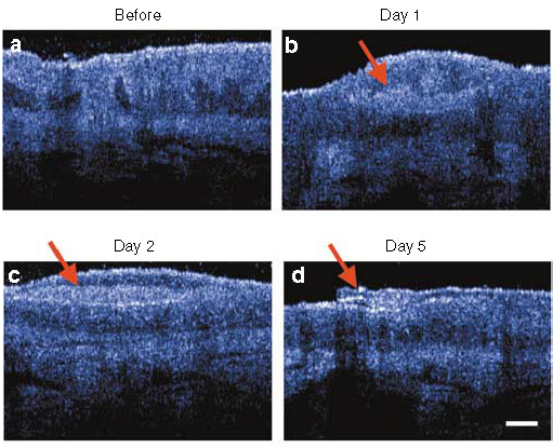
OCT image after the first treatment. The red arrow indicates the rapid migration of IEMC to the skin surface, and the epidermal thickness became thinner on the 5th day
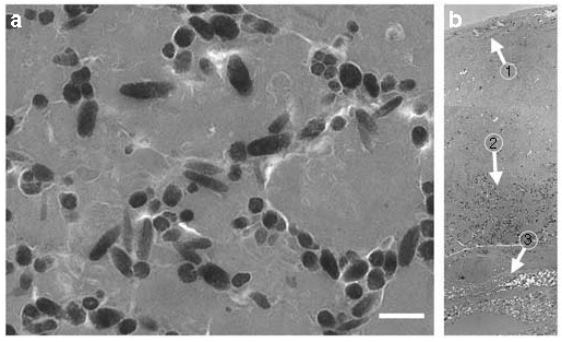
Electron microscopy imaging of IEM. Many melanosomes were observed in the exfoliated surface of sunspot skin. (a) Melanocytes in IEM. (b) Vertical cross-sectional images of IEM constructed from electron microscopy images. Arrows 1-3 represent the stratum corneum, melanosomes, and partially newly synthesized stratum corneum, respectively. From the results of this study, it can be concluded that the photothermal decomposition mechanism of intense pulsed light on pigmentary lesions includes promoting rapid differentiation of keratinocytes, accompanied by the upward transfer of melanosomes and necrotic keratinocytes, which leads to the elimination of melanosomes when clearing epidermal crusts on the skin, thereby treating superficial pigmentary lesions
II. Intense pulsed light therapy for post inflammatory pigmentation
Post inflammatory erythema (PIE) and post inflammatory hyperpigmentation (PIH) are the most common acne related sequelae. PIE is composed of telangiectasia and erythematous papules, which usually appear after the clearance of inflammatory acne. These vascular lesions are mainly located very close to the surface of the skin, and due to the presence of a small number of blood vessels in this area, the appearance is red.. PIH manifests as localized or diffuse brown to grayish brown spots in the affected area of acne, most pronounced after the disappearance of PIE. Xianglei Wu et al. [2] investigated the efficacy and safety of intense pulsed light therapy for acne related PIE and PIH.
This study recruited 60 patients with post acne PIE and PIH and treated them with intense pulsed light. Three filters were used sequentially during each treatment: 640nm filter (energy density 8-12 J/cm2, pulse width 30-35ms), 590nm filter (energy density 8-12 J/cm2, pulse width 15-20ms), and 560nm filter (energy density 6-10J/cm2, pulse width 12-15ms). The number of treatments is 3-7 times, with an interval of 4-6 weeks. Before each treatment and 6 months after the last treatment, the overall aesthetic improvement scale GAIS score, Cardiff Acne Disability Index CADI score, erythema assessment scale EAS score, and VISIA quantitative analysis were used to evaluate the efficacy of intense pulsed light therapy for post acne PIE and PIH
After treatment, the GAIS score showed that 49 out of 60 subjects (81.7%) had improved erythema and pigmentation.
; The CADI score has decreased significantly from an average of 9 points before treatment to an average of 7 points; The EAS score also significantly decreased.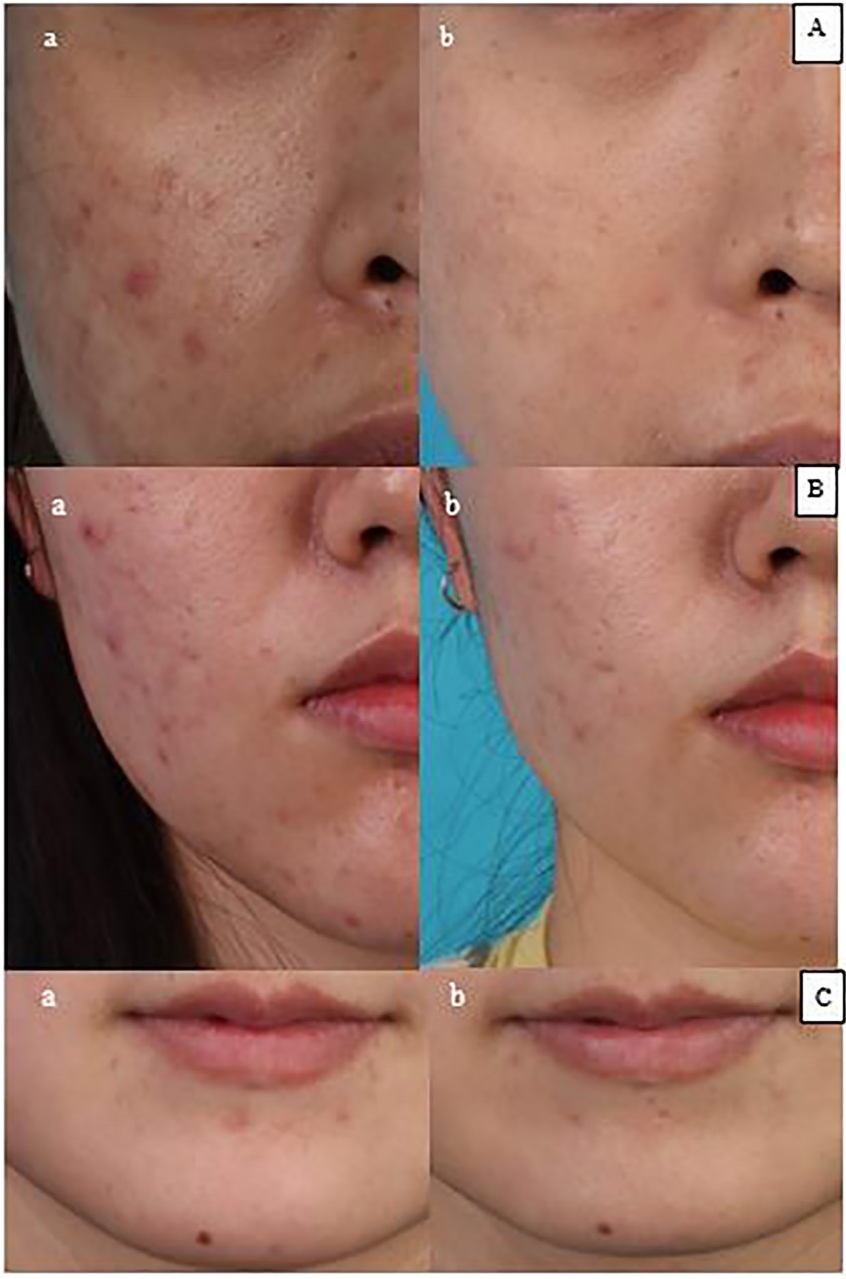
Photos before and after treatment show improvement in facial PIE and PIH
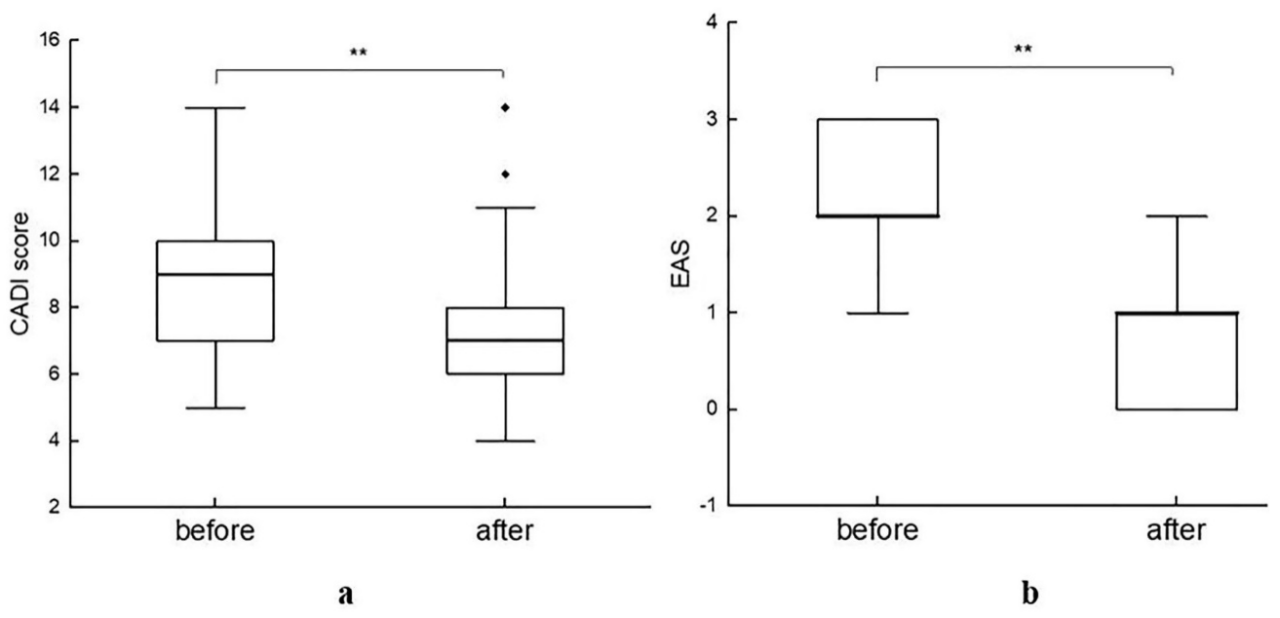
Changes in CADI and EAS scores, * * p<0.01]
Quantitative analysis was performed on the red area and brown spots on the face using VISIA before treatment and at the end of follow-up. These two features showed significant improvement after intense pulsed light therapy (p<0.01).
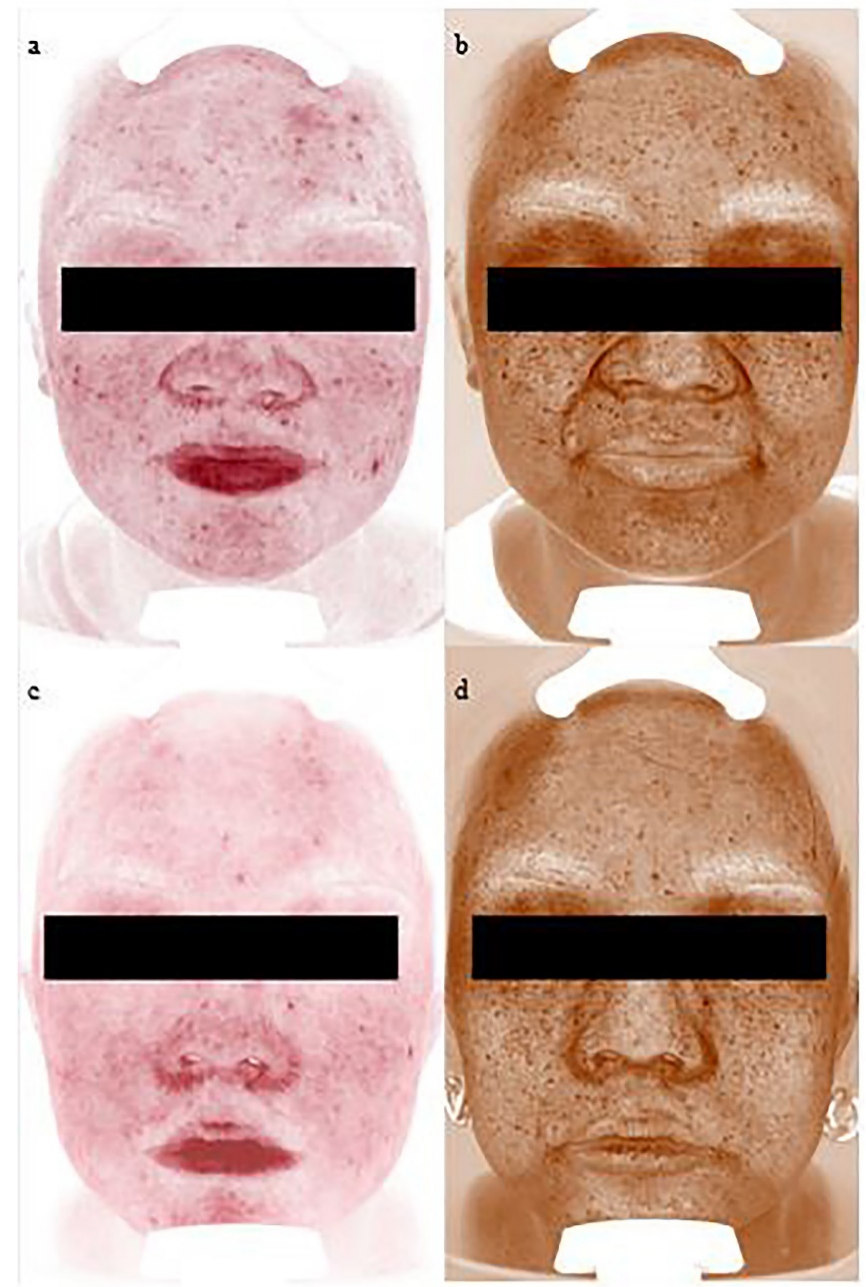
Comparison of VISIA images before treatment and at the end of follow-up
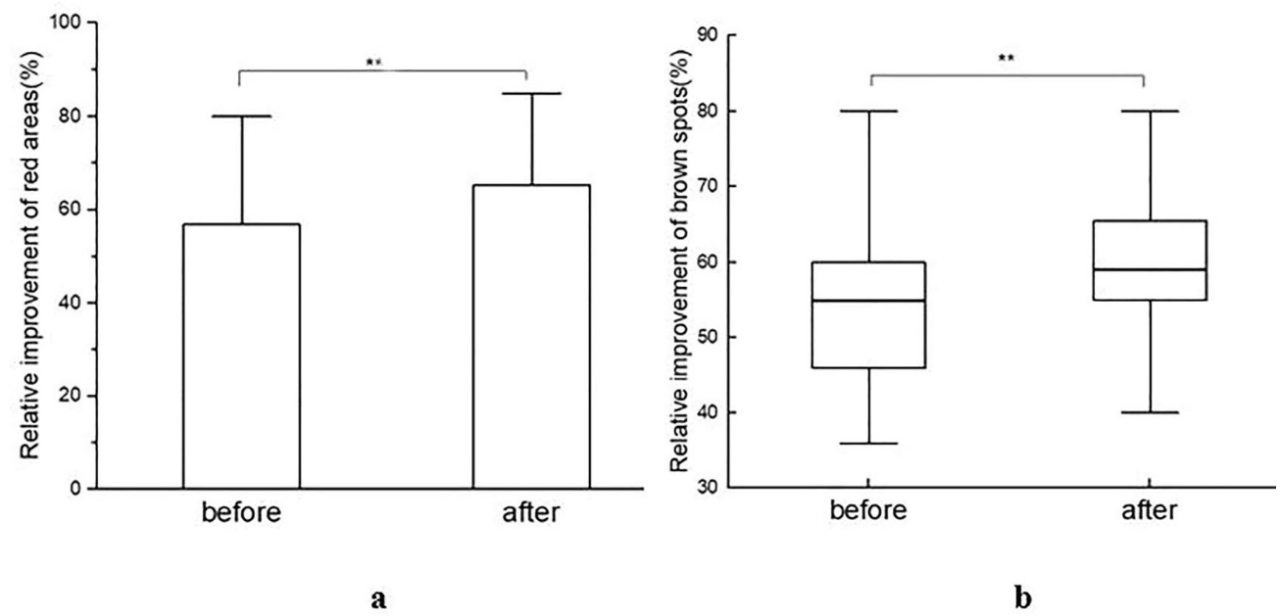
Red area (a) and brown spot (b) scores, * * p<0.01
3、 Summary
The strong pulse light therapy device is based on the theory of selective photothermal action, which allows melanocytes in the skin to absorb light energy, convert it into heat, undergo decomposition, migrate to the epidermis, and be excreted from the body, thereby achieving the goal of treating pigmentary skin diseases. During treatment, 560nm and 590nm filters, as well as appropriate parameters such as pulse width, number of sub pulses, and energy density, are usually selected based on the patient's skin type and lesion type, which have significant therapeutic effects.
Copyright © Suzhou Foremed Legend Technology Co., Ltd.